What are intracranial aneurysms?
Intracranial aneurysms are localized pathological dilatations of cerebral arteries. Most intracranial aneurysms are saccular or berry aneurysms, whereas dissecting, fusiform, infectious, traumatic, and oncotic aneurysms are much rarer. Saccular, or berry aneurysms, correspond to lobulated focal outpouchings of the wall of the arteries of the circle of Willis. Current opinions suppose that intracranial aneurysms result from a combination of hemodynamic stresses and acquired degenerative changes within the arterial wall
How does aneurysm presents?
Aneurysms may present as
- Rupture of the weak wall of such aneurysms mainly resulting in subarachnoid haemorrhage (SAH), experienced as ''the worst headache of life'' by patients.
- Mass effect, causing cranial nerve symptoms.
- Asymptomatic, incidentally detected during imaging done for other reasons.
- It is accepted that about 3% to 5% of the population harbour an intracranial aneurysm.
- One in every 20 strokes is caused by subarachnoid hemorrhage from rupture of intracranial aneurysm.
- Because the disease strikes a fairly young age and is often fatal the loss of productive life years is similar to that for cerebral infarction or intra cerebral hemorrhage.
What are complications of SAH?
Many patients don't survive initial hemorrhage or suffer significant brain injury due to the haemorrhage. Those who survive have high chance of repeat bleeding which can be fatal in as high as 70-80% of cases. Even if the aneurysm is repaired before rebleeding, 15% of patients who survive the initial hemorrhage develop ischemic strokes or die from the development of cerebral vasospasm. Non-Neurological Complications often occur in patients with SAH. These include fever, anemia, hypertension and hypotension, hyperglycemia, hypernatremia/hyponatremia, hypomagnesaemia, cardiac failure and arrhythmias, and pulmonary edema and pneumonia. Therefore these patients needs intensive care management so as avoid and mange such problems.
What are Diagnostic Recommendations?
- CT scan should be performed in suspected SAH. However, CT can be negative in some cases particularly if it is done few days after the event.
- Although MR is quite sensitive if performed appropriately and interpreted by an experienced radiologist, SAH is frequently missed
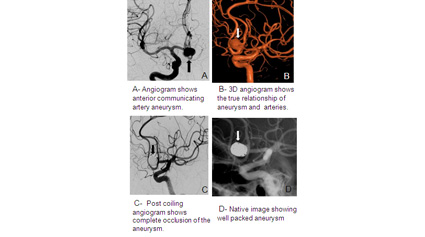
- Selective cerebral angiography should be performed in patients with SAH to document the presence and anatomic features of aneurysms
- MR angiography or CT angiography may be considered when conventional angiography cannot be performed in a timely fashion.
What Are Management Recommendations?
SAH is a medical emergency that is frequently misdiagnosed. A high level of suspicion for SAH should exist in patients with acute onset of severe headache. Patient of SAH are to be managed in ICU with good neuroanaesthetic support and management. Early aneurysm treatment should be performed to prevent repeat bleeding.
Surgery (clipping) vs embolization (coiling)
Surgery has been the conventional method of aneurysm treatment. Surgery entails direct exposure of the aneurysm, the parent vessel(s) and surrounding structures. The aneurysm is then secured by the placement of a metallic clip along the neck thereby excluding it from the circulation. Problems with surgery include invasiveness and trauma to normal brain parenchyma.
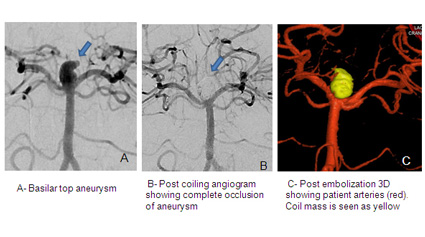
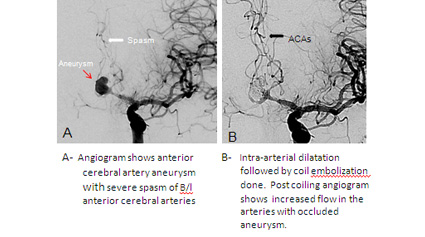
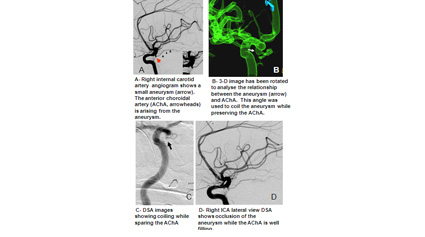
Other treatment option is of endovascular embolization (coiling) of Aneurysms. In this treatment a microcatheter is placed from one of the leg arteries in to the aneurysm, which is then occluded with coils (usually detachable platinum coils) so as to prevent repeat bleeding. Advantages: Since coiling is a minimally invasive technique it is less likely to result in injury to brain parenchyma. It is associated with
International Subarachnoid Aneurysm Trial Study (ISAT)
- Randomized, prospective, international controlled trial Compared policy of neurosurgical clipping with a policy of endovascular treatment in aneurysms deemed suitable for either therapy.
- 9559 patients screened, 2143 (22.4%) were randomized and the difference in the risk of dependency or death between the two groups was compared.
- Results: at 1 year, the outcome was much better in the coiling group with relative risk reduction of 22.6% as compared to surgical patients.
- The early survival advantage was maintained for up to 7-years.
- The risk of epilepsy was substantially lower in patients allocated to endovascular treatment. The risk of late rebleeding was minimally higher (0.16%). The better outcome in coiling group was inspite of minimally increased risk of rebleeding.
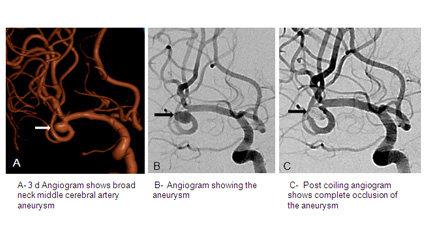
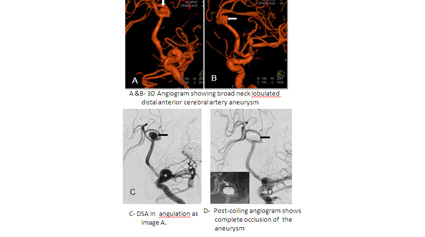
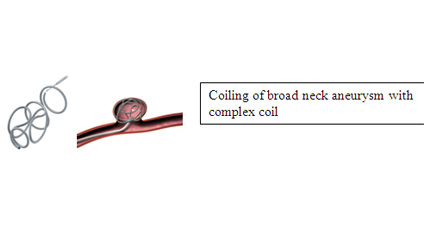
Are broad neck aneurysms amenable for coiling?
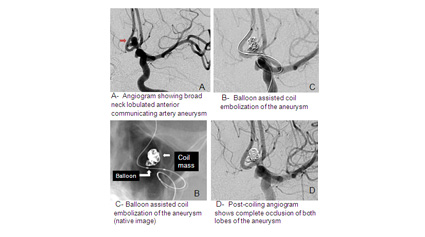
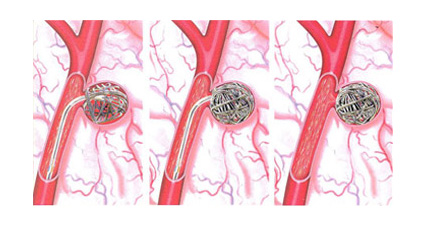
Most of the broad neck aneurysms can be treated by coiling, with use of 3D and complex coils. These coils are stable even in broad neck aneurysms. SAH is a medical emergency that is frequently misdiagnosed. A high level of suspicion for SAH should exist in patients with acute onset of severe headache. Patient of SAH are to be managed in ICU with good neuroanaesthetic support and management. Early aneurysm treatment should be performed to prevent repeat bleeding. Some cases require balloon assistance or stent placement Balloon assisted coiling for broad neck aneurysm- concept- a balloon is inflated temporarily at the neck of the aneurysm to hold the coils. Stent assisted coiling of broad neck aneurysm- a stent is placed across the neck of a broad neck aneurysm so as to hold the coils and reconstruct the artery
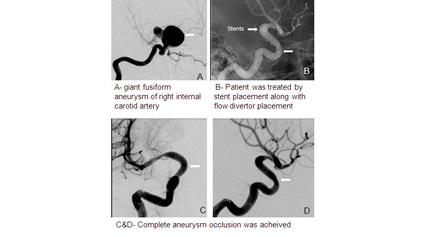
What are flow diverters? When do we use flow diverters?
Flow diverter is a stent with a more tightly woven wire mesh and therefore less porosity. Flow diversion is an endovascular technique whereby instead of placing a device inside the aneurysm sac, such as with coiling, the device is placed in the parent blood vessel to divert blood flow away from the aneurysm itself. This technique is used to unruptured treat large or giant wide-necked and very small ruptured blister like aneurysms . Almost immediately after stent deployment the blood flow to the aneurysm sac is reduced, and complete closure of the aneurysm occurs between 6 weeks to 6 months after the procedure.Flow diverter restores original, natural blood circulation while providing permanent long-term occlusion.